Understanding Liver Cancer: Causes, diagnostics, and therapeutic avenues
Written by Selin Dayan-Özdurmus, PhD researcher at German Cancer Research Center (DKFZ), Heidelberg
Liver cancer is a significant health concern worldwide, especially a challenge in the field of oncology, primarily hepatocellular carcinoma (HCC) and cholangiocarcinoma (CCA). Its incidence, prevalence, and prognosis vary across different demographics, highlighting the need for a comprehensive understanding.
Occurrence:
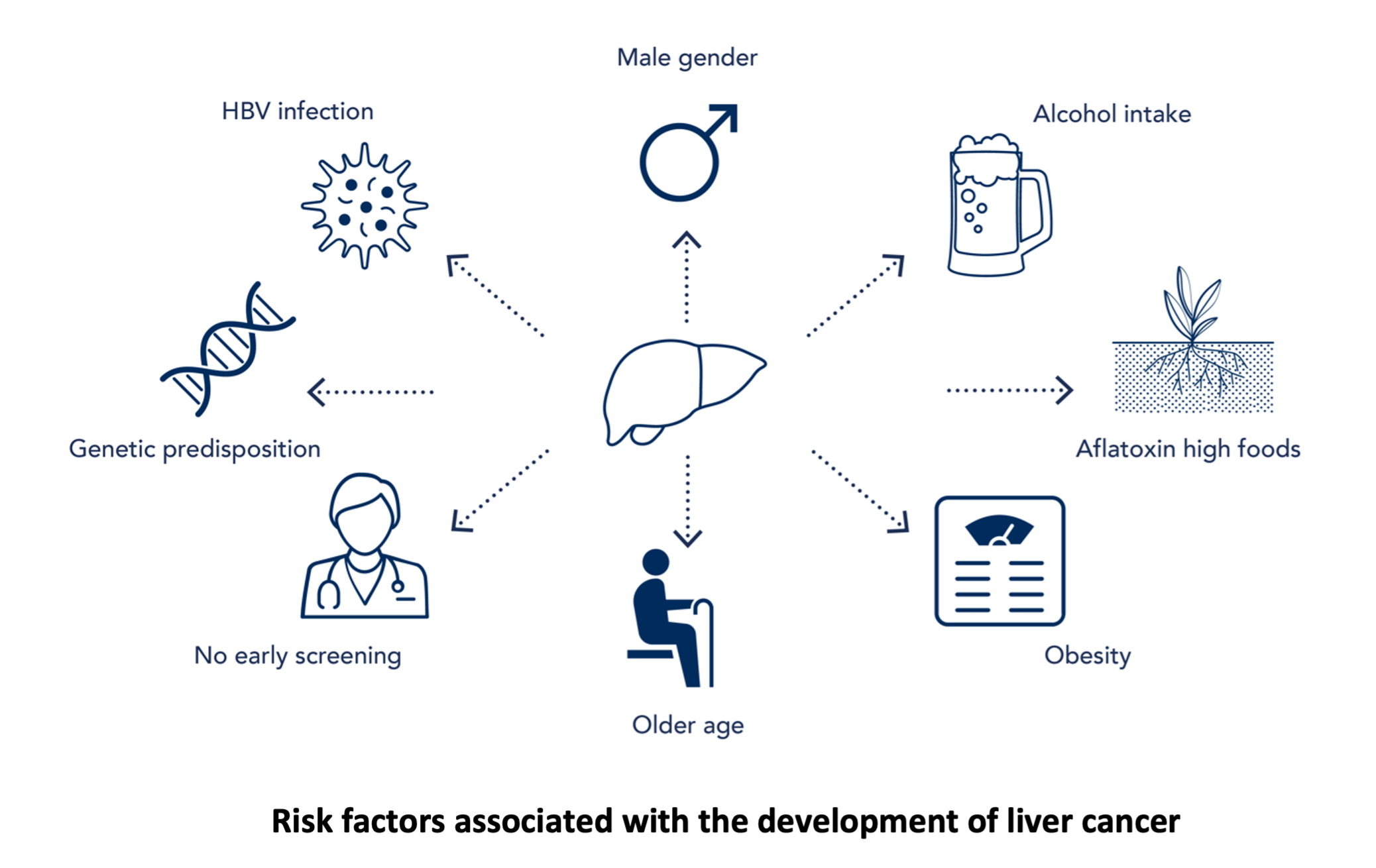
Liver cancer, predominantly hepatocellular carcinoma (HCC), can arise from factors such as chronic Hepatitis B (HBV) or Hepatitis C (HCV) infections, excessive alcohol intake, NAFLD (nonalcoholic fatty liver disease), and exposure to aflatoxins. However, its occurrence isn’t evenly distributed globally, with disparities seen in regions with endemic hepatitis infections, particularly parts of Asia and Africa.
In parts of Asia, chronic HBV infection is a major risk factor for liver cancer due to early exposure to the virus and inadequate access to vaccination programs. Similarly, in some African countries, endemic HBV and HCV infections contribute to a higher prevalence of liver cancer, worsened by socioeconomic factors and limited healthcare access.
Ethnic disparities also influence the risk of liver cancer, with certain groups like Asian and Pacific Islander populations showing higher rates due to genetic predispositions and cultural practices. To address these differences, targeted interventions such as comprehensive vaccination programs, improved screening, and efforts to reduce modifiable risk factors like alcohol consumption should be prioritized. By doing that, the global burden of liver cancer, and thus the outcomes for affected individuals, can be enhanced.
Gender differences:
Notably, there are also differences in liver cancer occurrence between genders. Historically, men have been shown to have a higher susceptibility to HCC compared to women. This discrepancy has been attributed to various factors, including different underlying risk factors such as HBV and HCV infections, as well as lifestyle behaviors and hormonal influences.
Lifestyle factors:
The development of liver cancer is linked to changeable lifestyle factors. Chronic alcohol consumption and obesity significantly heighten the risk of developing the disease. Excessive alcohol intake can lead to liver cirrhosis, a precursor to HCC. At the same time, obesity and metabolic syndrome contribute to the development of NAFLD, a growing cause of liver cancer globally. Dietary factors, like the consumption of food that is high in aflatoxins, further elevate the risk. Promoting healthy lifestyle habits that include reduced alcohol consumption, weight management, and a balanced diet is essential to decrease the risk of liver cancer.
Molecular markers:
Advancements in molecular biology have changed the way we understand liver cancer. Molecular markers offer important insights into the underlying molecular mechanisms driving hepatocellular carcinoma (HCC) and help guide clinical decision-making.
Alpha-fetoprotein (AFP):
- Alpha-fetoprotein (AFP) is one of the most well-known and widely used biomarkers for HCC. While high levels of AFP can be a sign of HCC, it is important to note that AFP alone lacks specificity and sensitivity. This is especially true for the early stage of the disease. Still, when combined with imaging like ultrasound, AFP can improve early detection of HCC and help monitor treatment response.
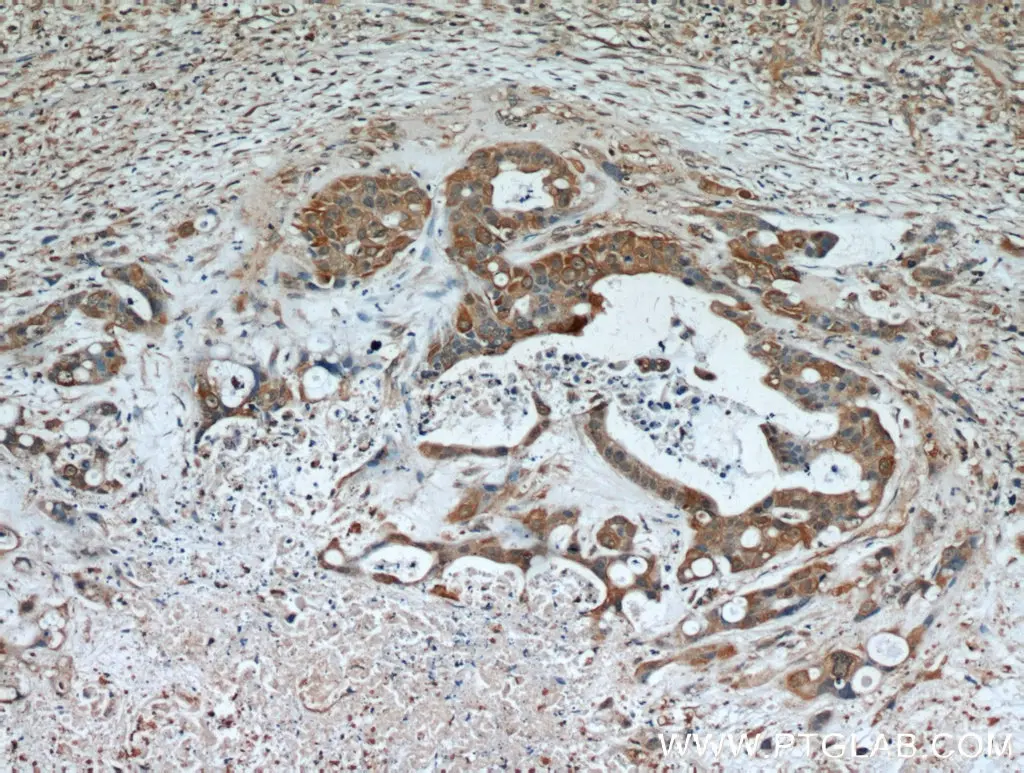
Glypican-3 (GPC3):
- GPC3 is a cell surface protein that is overexpressed in HCC cells. It serves as a biomarker for HCC diagnosis and prognosis. Studies have shown that GPC3 levels are elevated in HCC tissues compared to non-cancerous liver tissue, highlighting GPC3 as a biomarker for distinguishing between benign and malignant liver lesions [1]. Also, GPC3 expression has been associated with aggressive tumor behavior and poor prognosis in HCC patients.
Des-gamma-carboxy prothrombin (DCP):
- DCP, also known as protein induced by vitamin K absence or antagonist-II (PIVKA-II), is another biomarker used to diagnose and monitor HCC. DCP levels are higher in the serum of HCC patients, particularly those with advanced disease status. High DCP levels have been correlated with larger tumor size, vascular invasion, and poorer survival outcomes [2]. Like AFP, DCP is often used with imaging studies to improve HCC detection and management.
Further genetic mutations and alterations:
- Genetic mutations and alterations contribute to the development and progression of HCC. Characterizing specific genetic aberrations, such as mutations in the TP53, CTNNB1, and TERT genes, can give insights into prognosis and guide targeted therapies. For example, the presence of CTNNB1 mutations is associated with stronger disease progression, while mutations in the TERT promoter are associated with more aggressive tumor behavior.
MicroRNAs (miRNAs):
- MicroRNAs are small non-coding RNAs that are involved in gene expression. Dysregulation of miRNA expression has been implicated in various cancers, including liver cancer [3]. Specific miRNAs have been identified as potential biomarkers for HCC diagnosis, prognosis, and treatment response. For example, miR-21, miR-122, and miR-221 have been shown to be differently expressed in HCC and may serve as diagnostic or prognostic markers [4].
Circulating Tumor Cells (CTCs):
- Circulating tumor cells (CTCs) are cancer cells that have shed into the bloodstream from primary tumors and can serve as biomarkers for tumor progression and metastasis. Detection and characterization of CTCs in peripheral blood have shown to be valuable in following HCC patients' response to treatment and predicting disease recurrence [5]. Technologies such as immunomagnetic separation and microfluidic devices enable the capture and analysis of CTCs, providing insights into tumor biology and treatment efficacy.
In addition to their diagnostic and prognostic utility, molecular markers hold promise as therapeutic targets in HCC. Targeted therapies aimed at specific molecular pathways, such as the vascular endothelial growth factor (VEGF) and mammalian target of rapamycin (mTOR) pathways, have shown efficacy in HCC patients with specific biomarker profiles. Furthermore, immunotherapies targeting immune checkpoint molecules such as programmed cell death protein 1 (PD-1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) have demonstrated promising results in subsets of HCC patients, highlighting the potential of molecularly guided treatment approaches.
Conclusion:
Liver cancer remains a formidable challenge, characterized by its complex etiology, gender disparities, and profound impact on public health. Addressing the multifaceted determinants of liver cancer occurrence, including modifiable lifestyle factors and molecular markers, is imperative in advancing prevention, early detection, and treatment strategies. By fostering collaborative efforts between clinicians, researchers, and policymakers, we can strive towards a future where liver cancer is no longer a pervasive threat but rather a conquerable foe through comprehensive and targeted interventions.
References
[1]: Capurro, M., Wanless, I. R., Sherman, M., Deboer, G., Shi, W., Miyoshi, E., & Filmus, J. (2003). Glypican-3: a novel serum and histochemical marker for hepatocellular carcinoma. Gastroenterology, 125(1), 89–97.
[2]: Carr, B. I., Kanke, F., Wise, M., & Satomura, S. (2007). Clinical evaluation of lens culinaris agglutinin-reactive alpha-fetoprotein and des-gamma-carboxy prothrombin in histologically proven hepatocellular carcinoma in the United States. Digestive Diseases and Sciences, 52(3), 776–782.
[3]: Morishita A, Oura K, Tadokoro T, Fujita K, Tani J, Masaki T. MicroRNAs in the Pathogenesis of Hepatocellular Carcinoma: A Review. Cancers (Basel). 2021 Jan 29;13(3):514. : 10.3390/cancers13030514. PMID: 33572780; PMCID: PMC7866004.
[4]: Huang, P. S., Liao, C. J., Huang, Y. H., Yeh, C. T., Chen, C. Y., Tang, H. C., Chang, C. C., & Lin, K. H. (2021). Functional and Clinical Significance of Dysregulated microRNAs in Liver Cancer. Cancers, 13(21), 5361.
[5]: Salehi, M., Lavasani, Z. M., Keshavarz Alikhani, H., Shokouhian, B., Hassan, M., Najimi, M., & Vosough, M. (2023). Circulating Tumor Cells as a Promising Tool for Early Detection of Hepatocellular Carcinoma. Cells, 12(18), 2260.
Related Content
Support
Newsletter Signup
Stay up-to-date with our latest news and events. New to Proteintech? Get 10% off your first order when you sign up.