Second Cancer After Breast Cancer
Explore why breast cancer survivors are more likely to develop a second cancer after the first one has been cured.
A second cancer is different from a recurrence, which is when the same cancer returns after treatment, surgery, or cancer cell dormancy at distant organs – known as metastatic disease. A second cancer after breast cancer could be another breast cancer, perhaps originating in the other breast, or another type of cancer such as lung cancer, sarcoma, leukemia, or uterine cancer. Second cancers have become more common as people live longer and a higher proportion of people survive cancer.
What can cause a second cancer?
-
Genetic Factors: A mutation in the BRCA1/2 gene can significantly increase the risk of a second breast cancer, ovarian cancer, and other cancers. Other genetic risks such as Lynch syndrome and Familial Adenomatous Polyposis (FAP) can increase the risk of developing bowel cancer.
- Radiotherapy: Receiving ionizing radiation as treatment for your first breast cancer can increase the risk of developing lung cancer or sarcomas of bone and endothelial cells in the chest. Radiation can also weaken the immune system, leaving the body vulnerable to the development of cancer.
- Chemotherapy: The cytotoxic effects of chemotherapy, especially alkylating and platinum-based agents, can cause impaired hematopoiesis in the bone marrow. The resulting abnormal HSCs (hematopoietic stem cells) can lead to acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS). An increase has been reported in cytogenetic abnormalities as a result of chemotherapy, which is also associated with multiple forms of leukemia. Impaired hematopoiesis decreases the number of healthy HSCs, resulting in a weakened immune system incapable of stopping tumorigenesis.
- Tamoxifen: Although very effective against hormone-responsive breast cancer, Tamoxifen produces a three-fold increase in the risk of developing uterine or endometrial cancer.
Reducing the risk of a second cancer:
- Lifestyle changes: Cancer survivors have an increased chance of developing cancer compared to people of the same age and gender who have never had cancer. It is therefore very important to know the risk factors and take preventative lifestyle measures, such as regular exercise, a healthy diet, and avoiding smoking and alcohol intake.
- Preventative surgery: For those who have already had a first breast cancer or those with BRCA1/2 mutations, a preventative mastectomy can reduce the risk of a second breast cancer occurring.
- Proton beam radiotherapy: There have been significant improvements in radiotherapy with the use of lower doses and targeted delivery via technologies such as proton beam therapy. This uses protons rather than photons (x-ray) to deliver the ionizing effects at the end of the beam, sparing the peripheral tissue.
- Adjuvant therapy: Clinics have several hormone and targeted therapies available for breast cancer. This enables chemotherapy to be used at significantly lower doses, reducing the risk of developing hematologic malignancies.
Although it is impossible to dissociate the contribution of treatment or the first cancer to the development of a second cancer, studies have shown the risk of a second cancer is lower than the improvement in breast cancer mortality with chemo- and radiotherapy.
If a patient has had breast cancer, they will be closely followed to detect and track the potential early development of a second cancer. A rapid and non-invasive approach is via liquid biopsies using a blood or bone marrow sample. This will also detect any hematologic abnormalities, which can be early markers of AML or MSD.
We have listed below some of the markers used to detect or study second cancers after breast cancer.
CD34: Marker for hematologic disorders such as AML or MSD
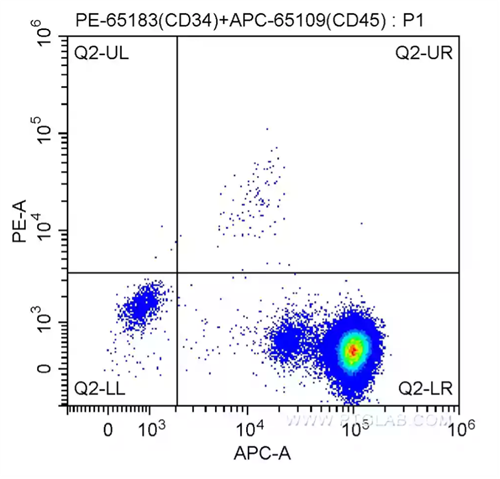
Fig. 1: 100 ul human peripheral blood was surface-stained with 20.00 ul PE Anti-Human CD34 (PE-65183, Clone: QBEnd-10) and 5 ul APC Anti-Human CD45 (APC-65109, Clone: HI30), and then treated with red blood cell lysis buffer. Cells were not fixed.
HLA-DR: Marker for hematologic disorders such as AML or MSD
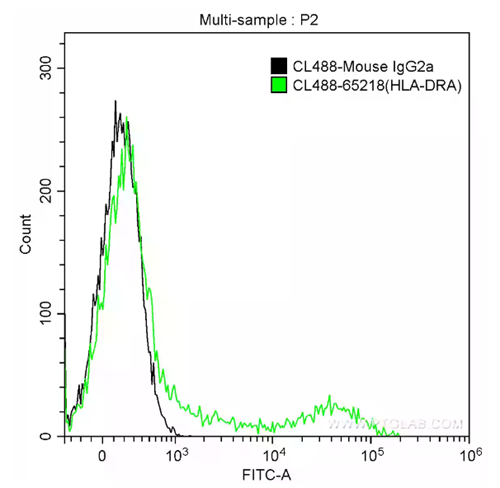
Fig. 2: 1X10^6 human peripheral blood lymphocytes were surface-stained with 5 ul CoraLite®488-conjugated Anti-Human HLA-DR (CL488-65218, Clone: L243) (green) or isotype control antibody (black). Cells were not fixed.
BRCA1/2: Genetic risk factor associated with breast and ovarian cancer

Fig. 3: Immunohistochemical analysis of paraffin-embedded human breast cancer slide using 22362-1-AP (BRCA1 Antibody) at dilution of 1:50.
CTLA4 and PDL-1: Biomarkers of tumor-associated immunosuppression
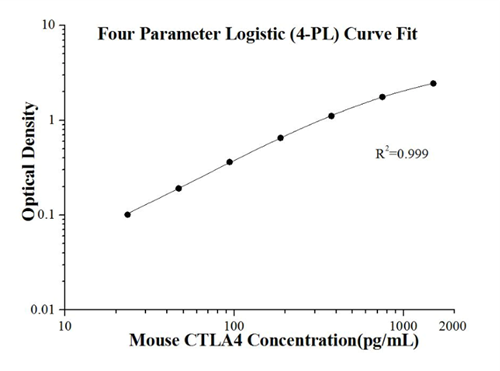
Fig.4 Standard curve of KE10029 Mouse CTLA4 ELISA Kit.
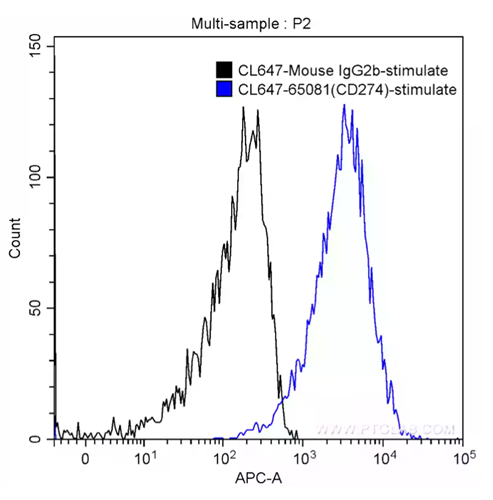
Fig. 5: 1X10^6 PHA-stimulated (5 ug/ml, 3 days) human peripheral blood lymphocytes were surface-stained with 5 ul CoraLite®647 Anti-Human PD-L1 (B7-H1) (CL647-65081, Clone: 29E.2A3) (blue) or isotype control (black). Cells were not fixed.
Blog written by Lucie Reboud, Intern at Proteintech, PhD student in cancer research at the University of Manchester.
References:
Matesich, S. M. A., & Shapiro, C. L. (2003, December). Second cancers after breast cancer treatment. In Seminars in oncology (Vol. 30, No. 6, pp. 740-748). WB Saunders.
Kirova, Y. M., De Rycke, Y., Gambotti, L., Pierga, J. Y., Asselain, B., & Fourquet, A. (2008). Second malignancies after breast cancer: the impact of different treatment modalities. British Journal of Cancer, 98(5), 870-874.
Malmgren, J. A., Calip, G. S., Pyott, S. M., Atwood, M. K., & Kaplan, H. G. (2016). Therapy-related myelodysplastic syndrome following primary breast cancer. Leukemia research, 47, 178-184.
Related Content
Cancer stem cells as a key to cure cancer
Support
Newsletter Signup
Stay up-to-date with our latest news and events. New to Proteintech? Get 10% off your first order when you sign up.